A rare case of hematologic peritonitis complicating secondary myelofibrosis
DOI:
https://doi.org/10.25796/bdd.v8i3.87085Keywords:
peritoneal dialysis, peritonitis, cloudy peritoneal dialysate, culture-negative peritonitis, secondary myelofibrosisAbstract
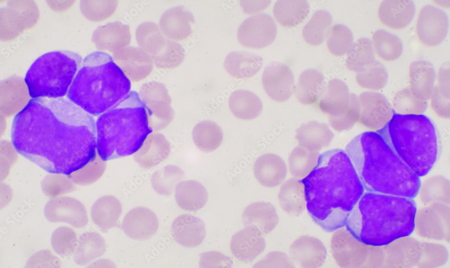
Peritonitis is a frequent complication of peritoneal dialysis. Its diagnosis is based on clinical signs (pain, cloudy effluent), intraperitoneal hyperleukocytosis (> 0.1×109/L with more than 50% polynuclears), or a positive culture. Although the majority of peritonitis cases are of infectious origin, there are also cases due to non infectious origin, which can lead to the inappropriate use of antibiotics and delayed diagnosis. We report the case of a 78-year-old male patient with a complex haemopathy that combined paroxysmal nocturnal haemoglobinuria, despite treatment with ravulizumab, and essential thrombocythemia, which transformed into myelofibrosis. After the initiation of peritoneal dialysis treatment, he presented with occasionally cloudy dialysis fluid rich in leukocytes (up to 0.442 ×10^9/L), with no evidence of infection (negative cultures and DNA16S PCR, moderate CRP, and an absence of atypical cells). The origin of the intraperitoneal hyperleukocytosis was attributed to myelofibrosis-related blood hyperleukocytosis. The clinical course was unfavorable, leading to palliative management.
This case illustrates the difficulty of managing this complication in peritoneal dialysis patients. Although infectious peritonitis is the most common first-line diagnosis, it is important to consider various differential diagnoses in cases of culture-negative peritonitis, particularly hematological causes (leukemia, lymphoma, myelofibrosis). However, forms with a predominance of neutrophils in the dialysate may simulate an infection. The absence of fever, elevated CRP, and a correlation between blood and peritoneal hyperleukocytosis should help in making a differential diagnosis. Immunophenotyping or molecular biology in the dialysate could refine the diagnosis. This case highlights a possible cause of sterile peritonitis due to myelofibrosis with hyperleukocytosis, and calls for recommendations to be adapted to increasingly complex clinical situations.
INTRODUCTION
Peritoneal dialysis is one of the techniques used for renal replacement therapy. It is commonly used in France, although much less than hemodialysis[1]. Like any technique, it is not without complications, the most well-known of which is peritonitis[2][3].
The diagnosis of peritonitis is based on the presence of at least two of the following[4]:
- clinical features consistent with peritonitis, i.e., abdominal pain or cloudy dialysis effluent;
- a white blood cell count in dialysis effluent > 100/µL or > 0.1 × 109/L (after a stasis time of at least 2 hours), with > 50% polymorphonuclear leukocytes (PMNs);
- a positive culture in the dialysis effluent.
The majority of peritonitis cases are infectious in origin, but other etiologies must be considered and investigated[5][6][7][8]. Signs of peritonitis are usually interpreted as infectious in origin to avoid delays in treatment, which can lead to significant morbidity and mortality. However, this can lead to complications, including the excessive use of antibiotics, which risks altering the bacterial ecology and promoting antibiotic resistance; it can also lead to delayed management of the underlying disease (which may be iatrogenic, an allergy, an oncological or hematological condition, or a surgical pathology). The recommendations for managing peritonitis [[4]] emphasize the need to initiate antibiotics promptly, given the potential severity of the infection; however, this recommendation must be qualified, and management must be adapted on a case-by-case basis.
Nephrology patients are often elderly, have multiple pathologies, and are on multiple medications. This presents us with a complex pattern of complications and observations, particularly in oncological and hematological contexts.
We report here a case of non-infectious peritonitis manifesting as sometimes cloudy peritoneal dialysis effluent, associated with an excess of intraperitoneal white blood cells secondary to blood hyperleukocytosis, itself a consequence of a hematological disease.
CASE PRESENTATION
A 78-year-old man developed stage V chronic kidney disease in the context of paroxysmal nocturnal hemoglobinuria that progressed despite treatment with ravulizumab (Ultomiris®, Alexion Pharma France) and then eculizumab (Soliris®, Alexion Pharma France). He had a history of paroxysmal nocturnal hemoglobinuria and also essential thrombocythemia with a cytogenetic diagnosis of MPL W515L and associated DNMT3A mutation, which secondarily transformed into myelofibrosis and had been treated with hydroxyurea (Hydrea®) and ruxolitinib (Jakavi®) since 2023 (with known hyperleukocytosis at 30G/L). He also presented with flutter and high blood pressure.
He began emergency extrarenal purification by hemodialysis after placement of a right internal jugular tunneled catheter on October 28, 2024, followed by peritoneal dialysis on January 6, 2025 (after placement of a peritoneal dialysis catheter accompanied by treatment for an inguinal hernia on December 9, 2024). His protocol included a short exchange (4 hours) of isotonic solution (Physioneal 40® with 1.36% glucose, Baxter International Inc.) and a long exchange of hypertonic solution (Extraneal®, Baxter International Inc.) for the rest of the nycthemeral cycle. The protocol was adapted to the patient's needs, his residual renal function, and the availability of registered nurses.
On January 13, 2025, his nurses reported difficulty with drainage and that the patient was suffering from abdominal pain. He was admitted to the day hospital and underwent an exchange, which restored the drainage fluid to a clear state. However, cytological examination revealed a white blood cell count of 0.139 × 109/L, with 53% polynuclear cells. Blood tests showed a CRP of 8 mg/L, a hemoglobin level of 9 g/dL, and a white blood cell count of 63 × 109/L, with 36 × 109/L of polynuclear cells.
Bacteriological samples of dialysis fluid and blood were cultured. The ASP found the catheter in place but with an accumulation of fecal matter. Because of the possibility of infectious peritonitis related to peritoneal dialysis, he was given empirical intraperitoneal antibiotic treatment with cefazolin and ceftazidime (in accordance with the Toulouse University Hospital protocol). Given his stable clinical condition, the patient was discharged home.
On January 14, 2025, he was re-evaluated in consultation due to persistent abdominal pain and slightly cloudy drainage fluid. Cytological examination revealed an elevated white blood cell count of 0.197 × 109/L, with 51% polymorphonuclear cells. He was admitted to the nephrology department on the same day.
Physical examination on admission showed no fever, a blood pressure of 160/80, and a heart rate of 70 bpm. Cardiopulmonary auscultation was normal. The abdomen was tender with no guarding or contracture. The results of laboratory and imaging tests after admission were as follows:
-Cytological analysis of the dialysis fluid revealed a white blood cell count of 0.201 × 109/L, with 29 % polynuclear cells.
- The effluent culture was negative, as was the 16S DNA (bacterial DNA by PCR),
-Blood te sts revealed a CRP of 4.4 mg/L, a hemoglobin level of 8.7 g/dL, and a white blood cell count of 67 × 109/L with a predominance of PNN.
-All blood cultures were negative.
-Computed tomography revealed parietal thickening of the colon associated with infiltration of peritoneal fat.
Given the results and despite no increase in CRP, a diagnosis of colitis without peritonitis was made, prompting a change in antibiotic therapy to intravenous tazocillin for a total duration of 7 days. The patient was discharged home.
On February 3, due to persistent asthenia, tests were performed to assess the progression of the patient's hematological disease:
-A myelogram showed poor
References
1. Réseau REIN. Synthèse du rapport annuel 2022 du réseau REIN [en ligne]. 2022 [cité le 1 mai 2025]. Disponible sur : https://www.agence-biomedecine.fr/fr/observatoire-de-la-maladie-renale-chronique/synthese-du-rapport-annuel-2022-du-rein-par-et-pour-les-patients-presentant-une-defaillance-renale-et-leurs-proches
2. Sahlawi, Muthana Al et al. “Peritoneal dialysis-associated peritonitis outcomes reported in trials and observational studies: A systematic review.” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 40,2 (2020): 132-140. doi:10.1177/0896860819893810
3. Marshall, Mark R. “A systematic review of peritoneal dialysis-related peritonitis rates over time from national or regional population-based registries and databases.” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 42,1 (2022): 39-47. doi:10.1177/0896860821996096
4. Li, Philip Kam-Tao et al. “ISPD peritonitis guideline recommendations: 2022 update on prevention and treatment.” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 42,2 (2022): 110-153. doi:10.1177/08968608221080586
5. Verger C, Veniez G, Dratwa M. Variability of aseptic peritonitis rates in the RDPLF. Bull Dial Domic [Internet]. 2018 Jun. 13 [cited 2022 Sep. 5];1(1):9-13. Available from: https://doi.org/10.25796/bdd.v1i1.30
6. Rocklin, M A, and I Teitelbaum. “Noninfectious causes of cloudy peritoneal dialysate.” Seminars in dialysis vol. 14,1 (2001) : 37-40. doi:10.1046/j.1525-139x.2001.00012.x
7. Teitelbaum, Isaac. “Cloudy peritoneal dialysate: it’s not always infection.” Contributions to nephrology vol. 150 (2006): 187-194. doi:10.1159/000093594
8. Cheng, Xin Bo Justin, and Joanne Bargman. “Complications of Peritoneal Dialysis Part II: Nonmechanical Complications.” Clinical journal of the American Society of Nephrology: CJASN vol. 19,6 (2024): 791-799. doi:10.2215/CJN.0000000000000418
9. Verger C, Fabre E, Veniez G, Padernoz MC. Données statistiques synthétiques du Registre de Dialyse Péritoneale de Langue Française et Hémodialyse à Domicile (RDPLF) en 2018. Bull Dial Domic [Internet]. 10avr.2019 [cité 12nov.2020];2(1):1-10.
10. De Freitas DG, Gokal R. Sterile peritonitis in the peritoneal dialysis patient. Perit Dial Int. (2005) : 146-51.
11. Yang, C C et al. “Splenic infarction: an unrecognized cause of culture-negative peritonitis in a continuous ambulatory peritoneal dialysis patient.” Clinical nephrology vol. 68,4 (2007) : 262-5. doi:10.5414/cnp68262
12. Nandagopal, L et al. “Sterile peritonitis because of splenic infarction in a patient on peritoneal dialysis: an unusual presentation.” Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis vol. 33,3 (2013): 339-40. doi:10.3747/pdi.2012.00139
13. Masaki, Chiaki et al. “Splenic abscess diagnosed following relapsing sterile peritonitis in a peritoneal dialysis patient: A case report with literature review.” Seminars in dialysis vol. 34,3 (2021): 245-251. doi:10.1111/sdi.12953
14. Manga, Farhabanu et al. “Acute pancreatitis in peritoneal dialysis: a case report with literature review.” European journal of gastroenterology & hepatology vol. 24,1 (2012): 95-101. doi:10.1097/MEG.0b013e32834d4bcc
15. Osaki, Yosuke et al. “Peritoneal dialysis-associated peritonitis, caused by superior mesenteric artery thrombosis with intestinal necrosis: a case report.” CEN case reports vol. 14,1 (2025): 1-5. doi:10.1007/s13730-024-00894-y
16. Chen, Chih-Wei et al. “Intestinal goblet cell carcinoid presenting with recurrent sterile peritonitis in a patient on peritoneal dialysis: a case report.” BMC nephrology vol. 18,1 62. (2017) doi:10.1186/s12882-017-0477-x
17. Streather, C P et al. “Carcinoma of the kidney presenting as sterile peritonitis in a patient on continuous ambulatory peritoneal dialysis.” Nephron vol. 58,1 (1991) : 121. doi:10.1159/000186395
18. Jobson, V W, and P L Adams. “Endometrial carcinoma diagnosed by examination of peritoneal dialysate.” Obstetrics and gynecology vol. 62,2 (1983) : 264-6.
19. Akimoto, Tetsu et al. “Peritoneal Dialysis and Malignancy: An Experience With a Patient Complicated by Gastric Carcinoma.” Clinical medicine insights. Case reports vol. 12 1179547619835176. (2019) doi:10.1177/1179547619835176
20. Vlahakos, D et al. “Lymphoma-mimicking peritonitis in a patient on continuous ambulatory peritoneal dialysis (CAPD).” Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis vol. 10,2 (1990) : 165-7.
21. Bargman, J M et al. “Diagnosis of lymphoma in a continuous ambulatory peritoneal dialysis patient by peritoneal fluid cytology.” American journal of kidney diseases: the official journal of the National Kidney Foundation vol. 23,5 (1994) : : 747-50. doi:10.1016/s0272-6386(12)70289-5
22. Delgado-Córdova, Margarita et al. “Non-Hodgkin lymphoma mimicking peritonitis in a patient on peritoneal dialysis.” Nefrologia : publicacion oficial de la Sociedad Espanola Nefrologia vol. 34,5 (2014): 686-7. doi:10.3265/Nefrologia.pre2014.Apr.12386
23. Viray, Paul et al. “Hodgkin’s Lymphoma Diagnosed from Peritoneal Effluent.” Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis vol. 36,3 (2016): 350-1. doi:10.3747/pdi.2015.00119
24. Sriperumbuduri, Sriram, and Deborah Zimmerman. “Cloudy Dialysate as the Initial Presentation for Lymphoma.” Case reports in nephrology vol. 2018 2192043. 9 Oct. 2018, doi:10.1155/2018/2192043
25. Vigil, Darlene et al. “Noninfectious Cloudy Peritoneal Effluent in a Peritoneal Dialysis Patient with Mantle Cell Lymphoma.” Cureus vol. 10,10 e3413. (2018) doi:10.7759/cureus.3413
26. Vannucchi AM, Kantarjian HM, Kiladjian JJ, et al. A pooled analysis of overall survival in COMFORT-I and COMFORT-II, 2 randomized phase III trials of ruxolitinib for the treatment of myelofibrosis. Haematologica. (2015) : 1139-45. doi:10.3324/
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Charlotte Gabilan

This work is licensed under a Creative Commons Attribution 4.0 International License.








